A clinical pharmacist and health coach-delivered mobile health intervention can improve blood glucose levels in African American and Latinx populations, according to a study published […]
A review of performance measures for osteoporosis finds gap in measuring early treatment
A review of current performance measures that are applied to evaluate quality of osteoporosis care found that of the six osteoporosis performance measures relevant to […]
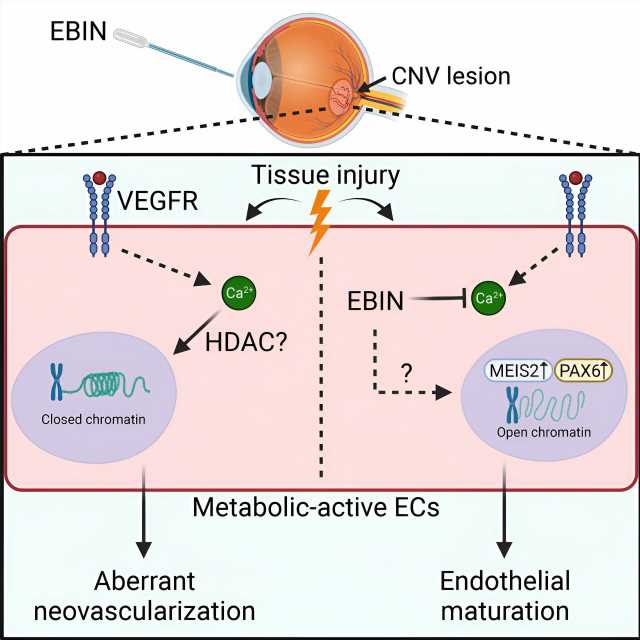
New strategy for eye condition could replace injections with eyedrops
A new compound developed at the University of Illinois Chicago potentially could offer an alternative to injections for the millions of people who suffer from […]
What Is the Future for Multicancer Early Detection Tests?
PARIS — Multicancer early detection blood (MCED) tests are the focus of intensive development. What techniques do these tests use? What potential do they show? […]
HIV self-test kits are meant to empower, but they don’t necessarily lead to HIV treatment or prevention
HIV self-test kits were developed to make it easier for people to access HIV testing. However, our research team has found that many people who […]
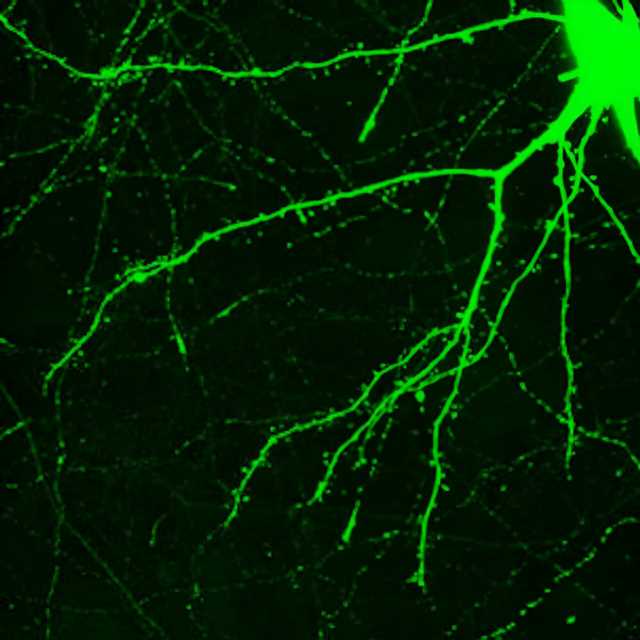
Psychedelics plus psychotherapy can trigger rapid changes in the brain: New research is untangling how
The human brain can change—but usually only slowly and with great effort, such as when learning a new sport or foreign language, or recovering from […]
Eli Lilly to buy cancer-focused Point Biopharma for $1.4 billion
FILE PHOTO: An Eli Lilly and Company pharmaceutical manufacturing plant is pictured at 50 ImClone Drive in Branchburg, New Jersey, March 5, 2021. Picture taken […]
Dr Michael Mosley recommends popular salad staple to ‘prevent cancer’
Cancer symptoms: Top 14 early signs to look out for It is thought around one in two people in the UK will develop cancer in […]
Joint injections ineffective for hand osteoarthritis symptoms, finds evidence review
Source: Read Full Article
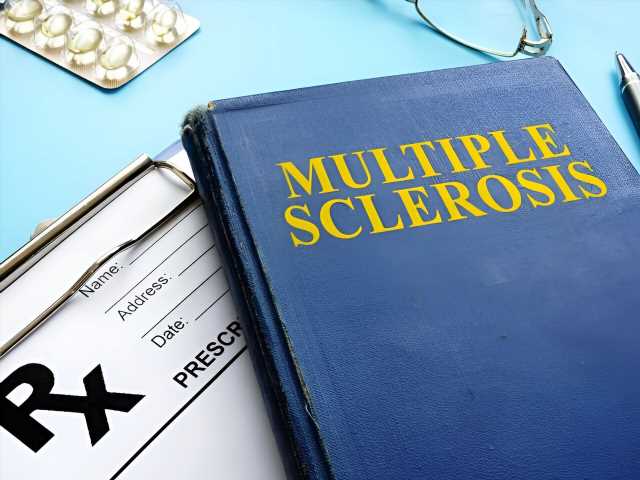
Stem cell treatment halts MS for some patients
A new study is strengthening the evidence that stem cell transplants can be highly effective for some people with multiple sclerosis—sending the disease into remission […]
Banning junk food won't stop people eating it says Dr Michael Mosley
DR MICHAEL MOSLEY: Banning junk food won’t stop people eating it, just look at how Prohibition failed! But we DO need new regulations to tackle […]
Support Tool Reduces Hypoglycemia Risk in Type 2 Diabetes
TOPLINE: Use of a novel clinical-decision support tool and shared decision making in elderly patients with type 2 diabetes managed in a primary care practice […]
Group practice sees 6-8 more patients a day with hybrid virtual care
Photo: Awab Sattar Dr. Richard Tytus of Hamilton, Ontario, is a medical professional with extensive experience in delivering and promoting virtual healthcare. He has been […]
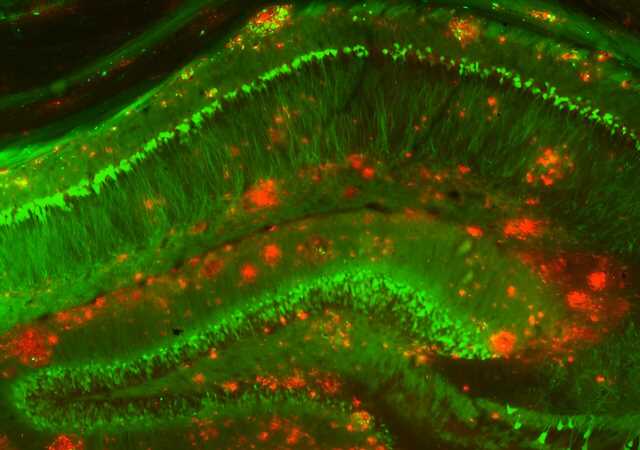
Scientists reveal cellular changes unique to early Alzheimer’s disease
Most Alzheimer’s disease research on human brain tissue has studied postmortem samples, making it difficult for scientists to discern the earliest events in the brain […]