Multiple sclerosis (MS) is a chronic inflammatory autoimmune disease in which the Epstein-Barr virus (EBV) is thought to play a role that has not yet […]
Enabling early detection of cancer with AI-based chromatin biomarkers
The ability to detect a developing tumor at a very early stage and to closely monitor the success or failure of cancer therapy is crucial […]
This next generation blue light could potentially promote or hinder sleep on command
Blue light from LED lamps and consumer electronics can mess with your sleep because it disrupts production of the natural sleep hormone melatonin. Tinted glasses […]
Research reveals novel ways of cultivating brain cells to treat and study
Scientists from Duke-NUS Medical School and their collaborators have come up with new methods to cultivate brain cells from stem cells to treat and study […]
Researchers develop ‘potent and specific’ compounds to curb cancer growth
Proteasomes are protein-degrading complexes that are important for cancer cell survival. Proteasome inhibitors are commonly used to treat diseases such as multiple myeloma and mantle […]
Almost ALL grapes and peaches sold in UK contain pesticide 'cocktail'
Almost ALL peaches, grapes and strawberries sold in UK contain a ‘cocktail of pesticides’ as research singles out ‘dirty dozen’ fruit and veg Analysis found […]
Deep neural networks show promise as models of human hearing
Computational models that mimic the structure and function of the human auditory system could help researchers design better hearing aids, cochlear implants, and brain-machine interfaces. […]
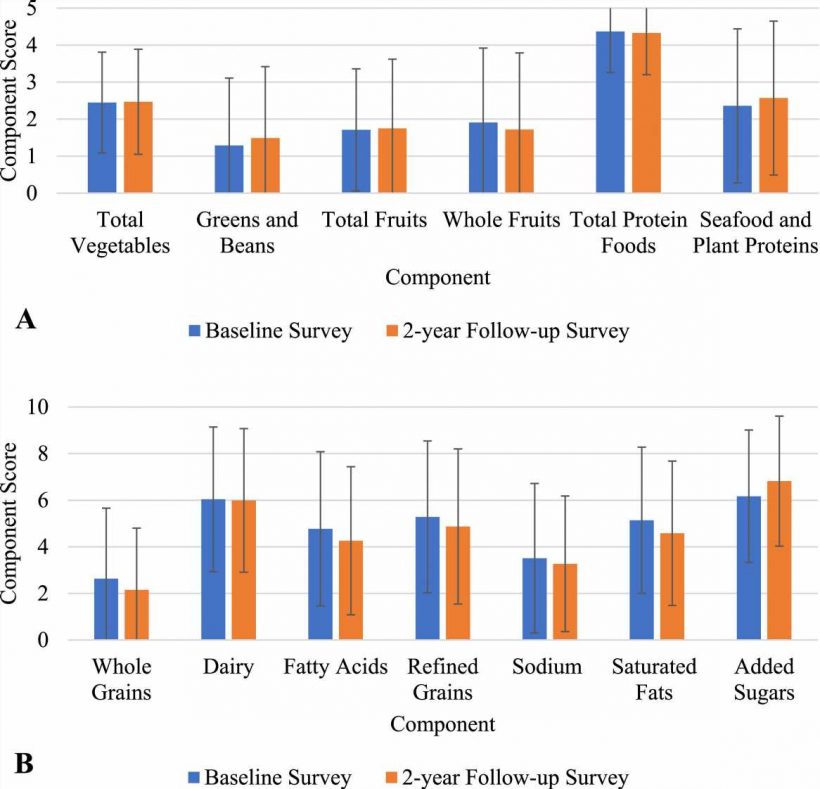
Poor diet quality during adolescence is linked to serious health risks
Diet quality among adolescents in the United States is among the worst across all age groups, putting young people at risk for heart attack, stroke, […]
Climate change risks triggering a spike in infectious disease outbreaks: three reasons why
Climate change is our planet’s most immediate existential threat, and will likely only worsen for the foreseeable future. Among its numerous adverse effects on human […]
Millions in opioid settlement funds sit untouched as overdose deaths rise
Reviewed Nearly a year after Montana began receiving millions of dollars to invest in efforts to combat the opioid crisis, much of that money remains […]
Patients can interrupt immune-suppressing medicines to boost immunity provided by COVID-19 booster, finds study
A major clinical trial, led by experts at the University of Nottingham, has shown that people with inflammatory conditions are able to improve the antibody […]
High BMI in adolescence linked to early chronic kidney disease in young adulthood
High body mass index (BMI) in late adolescence is associated with early chronic kidney disease (CKD) in young adulthood, according to a study published online […]
Coffee and caffeine boost metabolism and enhance exercise performance, study finds
In a recent study published in the journal Nutrients, researchers reviewed the effects of coffee and caffeine on metabolism and exercise. Coffee beverages represent the […]
People less likely to buy food when labeled as 'plant-based'
Don’t say vegan: People less likely to buy any food when labeled as ‘plant-based’, study finds When a food gift basket was labeled ‘vegan’ only […]