Off-label use of antidementia agents by patients with dementia with Lewy bodies (DLB) is linked to lower mortality, new research suggests.
Investigators found that among patients with DLB who used acetylcholinesterase inhibitors (AChEIs) and memantine off label, mortality rates were lower and hospital stays were shorter following unplanned hospitalizations for other medical conditions.
“Our findings provided new evidence for the possible benefits of AChEI treatment for those with DLB and suggest corresponding randomized controlled trial studies,” study investigators led by Shanquan Chen, MD, University of Cambridge, United Kingdom, write.
There are no approved treatments for DLB, the second most common form of neurodegenerative dementia in people over 65 after Alzheimer’s disease (AD). The standard treatment includes the off-label use of antidementia drugs, such as AChEIs and memantine.
Despite their widespread use for DLB, research on the drugs’ effectiveness in reducing mortality for these patients was scarce, although prior studies had suggested benefits for patients with AD and Parkinson’s disease dementia.
The findings were published online December 6 in PLOS Medicine.
Significant Benefit
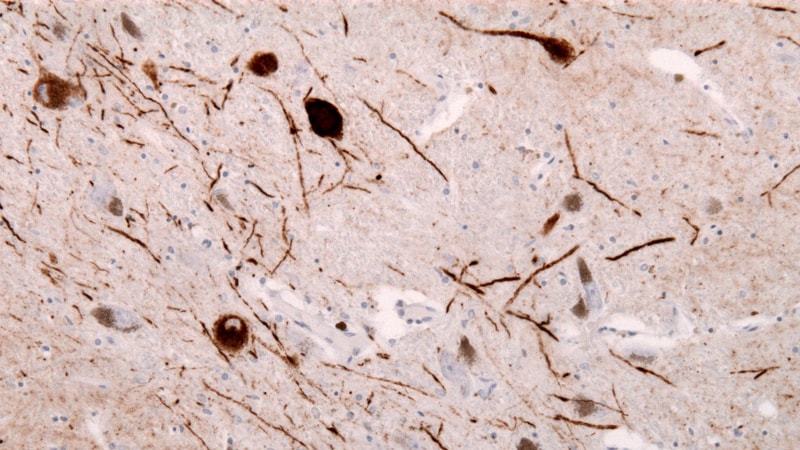
Patients with DLB may experience visual hallucinations and changes in alertness and attention. Other symptoms mirror muscular and movement problems that are common in Parkinson’s disease, including rigid muscles, slow movement, walking difficulty, and tremors.
Compared to AD, DLB is associated with accelerated cognitive decline, higher mortality rate, lower quality of life, and higher healthcare costs, as well as increased rates of hospital admissions and longer length of stay.
For the retrospective cohort study, researchers analyzed hospitalization and mortality data of 592 patients with DLB, including people who took AChEIs only (n = 100), people who took AChEIs plus memantine (n = 273), and patients who had never taken either drug (n = 219). The cohorts were followed up for an average of 896 to 1004 days.
Socioeconomic status was significantly lower for patients who had never taken either drug (P = .003).
After adjusting for age, sex, socioeconomic status, antidepressant or antipsychotic use, and other factors, mortality risk was significantly lower among patients who took AChEIs only (adjusted hazard ratio [aHR], 0.67; P = .02) or AChEIs plus memantine (aHR, 0.64; P = .001) compared to those who never took either drug.
Among those who took AChEIs alone or in combination with memantine, hospital stays during unplanned hospitalizations for physical disorders were significantly shorter (P = .049, P = .007, respectively).
Although the antidementia drugs were associated with higher rates of hospital admission for mental health disorders in adjusted models, once the researchers adjusted for a range of confounders, the association was no longer significant.
There was no difference in length of stay for planned admissions for physical disorders or for admissions for mental health disorders.
A “Noteworthy” Study
Commenting on the findings for Medscape Medical News, Melissa Armstrong, MD, director of the Dorothy Mangurian Clinical-Research Headquarters for Lewy Body Dementia at the University of Florida in Gainesville, described the study as “noteworthy with very important findings.
“The fact that cholinesterase inhibitors are associated with shorter duration of hospitalization and a decreased risk of mortality in DLB is critical,” she added.
However, she noted, the study didn’t allow for analysis of the dose-response relationship or distinguish between different types of AChEIs. There were also limitations inherent in retrospective studies with naturalistic design.
“While naturalistic studies have limitations, such as selection bias from nonrandom prescribing, this setting is also a strength, as it represents real-life scenarios,” Armstrong added. “It is notable that socioeconomic status was lower in patients who never took AChEIs or memantine, suggesting there are healthcare disparities in DLB that need to be addressed.”
The study was funded by the NIHR Cambridge Biomedical Research Centre and the Cambridge Centre for Parkinson’s Plus. Full disclosures for the study authors can be found in the original article. Armstrong has disclosed no relevant financial relationships.
PloS Med. Published online November 6, 2022. Full text
Kelli Whitlock Burton is a reporter for Medscape Medical News covering neurology and psychiatry.
For more Medscape Neurology news, join us on Facebook and Twitter.
Source: Read Full Article