An earlier first birth, a higher number of live births, and starting periods at a younger age are all linked to a higher risk of cardiovascular problems in women, according to new research.
The study, led by Imperial College London researchers, provides evidence for a causal relationship between sex-specific factors and cardiovascular disease in women, and identifies potential ways to mediate this increased risk.
The study is the most comprehensive analysis to date of reproductive factors specific to women and their links to a range of cardiovascular diseases, including atrial fibrillation (irregular heart rate), coronary heart disease, heart failure, and stroke. The researchers hope it will help doctors to better understand and monitor women’s risk factors and intervene where appropriate.
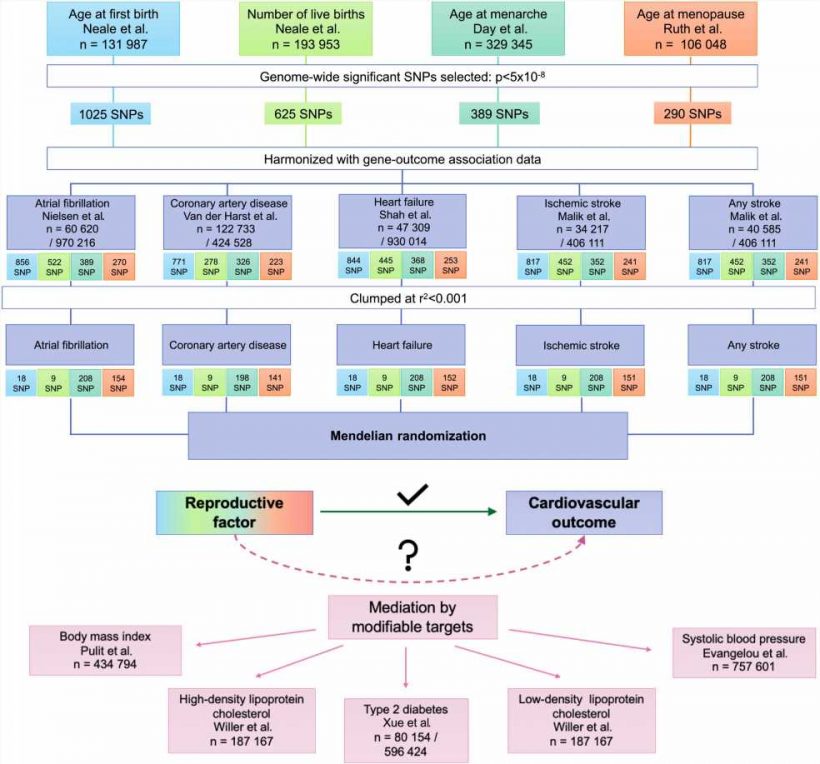
Researchers from Imperial’s National Heart & Lung Institute, University of Cambridge and Yale School of Public Health analyzed genetic data linked to women’s age at first birth, their number of live births, their age at their first period (menarche), and their age at menopause. They looked at previous studies involving more than 100,000 women.
Observational research has previously identified that some reproductive factors are associated with cardiovascular disease for women in later life, but such studies are limited as they have been unable to support a causal relationship.
By using a statistical technique called Mendelian Randomization, the researchers were able to show a link between the genes that predict reproductive factors and the risk of multiple cardiovascular diseases. This type of analysis enables researchers to cut through the noise of factors such as diet, economic background and physical activity levels that can otherwise complicate the overall picture, and so it points to causal links.
The analysis showed that earlier first birth, a higher number of live births, and earlier menarche were associated with a higher risk of atrial fibrillation, coronary artery disease, heart failure, and stroke in women. However, it did not find an association between the age of menopause and cardiovascular disease.
The researchers also found that much of the increased risk for earlier menarche resulted from this factor being associated with women having a higher body mass index (BMI). This means that lowering a person’s BMI could help to reduce this risk. The increased risk for earlier first birth could be partly limited by acting on traditional cardiometabolic risk factors, such as BMI, high cholesterol and high blood pressure.
Dr. Maddalena Ardissino, lead author of the study, from the National Heart and Lung Institute at Imperial College London, said, “Women are often mischaracterized as being at low risk for cardiovascular disease, leading to delays in diagnosis. Even when they are diagnosed, they tend to receive less targeted treatment than men.”
“This study shows a clear link between reproductive factors and cardiovascular disease. This doesn’t mean that women should worry if they’ve had their period at a young age, or if they had an early first birth. Our research shows that the additional risk of cardiovascular disease can be minimized if traditional risk factors like BMI and blood pressure are well-controlled. These findings highlight the need for doctors to monitor these risk factors closely in women and intervene where needed.”
Dr. Fu Siong Ng, senior author for the study, from the National Heart and Lung Institute at Imperial College London, said, “Many of the previous studies on cardiovascular disease have focused on men, but our research shows that there are sex-specific factors that influence the risk for women.”
“While we cannot say exactly how much these factors increase the risk of cardiovascular disease, our study shows that reproductive history is important and it points towards a causal impact. We need to understand more about these factors to make sure that women get the best possible care.”
Further research is needed to understand the extent of the relationship between reproductive factors and cardiovascular disease risk, such as whether there is a linear or non-linear relationship between a factor and increased risk.
Cardiovascular disease has often been thought of a man’s disease, as men are more likely to develop it at an earlier age than women. However, this group of diseases is a serious problem for women.
Research by the British Heart Foundation has shown that coronary heart disease kills more than twice as many women as breast cancer in the UK each year, with more than 800,000 women in the UK living with the disease. It is also estimated that around 380,000 women alive in the UK today have survived a heart attack.
Dr. Sonya Babu-Narayan, Associate Medical Director at the British Heart Foundation and consultant cardiologist, said, “The misconception that cardiovascular disease mostly affects men is costing women their health, and even their lives.”
“It’s critical that women are empowered with the knowledge of what could put them at higher risk of developing heart disease or stroke in the future. This includes the well-known risks that affect everyone—but for women, there may be additional risk factors from their reproductive years to add to the list.”
“If we’re going to save more women’s lives, asking about periods and pregnancy must be routine when assessing every woman’s risk of heart disease and stroke.”
The work is published in the Journal of the American Heart Association.
More information:
Maddalena Ardissino et al, Sex‐Specific Reproductive Factors Augment Cardiovascular Disease Risk in Women: A Mendelian Randomization Study, Journal of the American Heart Association (2023). DOI: 10.1161/JAHA.122.027933
Journal information:
Journal of the American Heart Association
Source: Read Full Article