Hypertension, commonly referred to as high blood pressure, is a non-communicable disease that occurs when there is a sustained elevation in the pressure of the blood that flows through the arteries.
Adults in low- and middle-income countries account for around 75% of the global cases.
High blood pressure is a manageable condition through regular monitoring, lifestyle changes and treatment. However, untreated blood pressure, also known as uncontrolled hypertension, can lead to damage to organs such as the kidneys, heart and brain. All this increases the risk for heart attack, stroke and other serious health issues.
Globally, uncontrolled hypertension is a leading contributor to death.
In Kenya, the 2014-2015 national survey on non-communicable diseases showed that high blood pressure contributed to a significant burden of disease. About one in four people have high blood pressure in the country. The hypertension prevalence for Kenya (24.5%) is slightly lower than that of neighboring countries such as Tanzania (26%) and Uganda (26.4%).
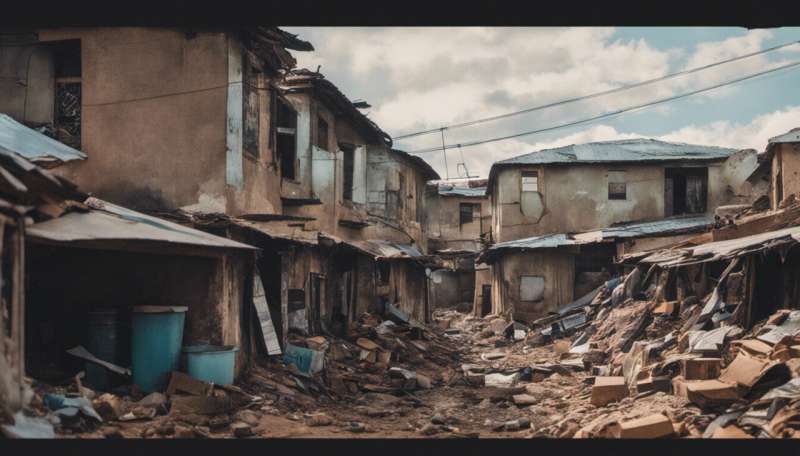
Research suggests that urban slum residents are 35% more likely to be hypertensive than people living in rural areas. In Nairobi, Kenya’s capital city, around 60% of the population lives in slums or slum-like conditions. Previous research in Kenya’s urban slums shows high uncontrolled hypertension rates.
In our recent study, my colleagues and I wanted to understand the range of factors that put these people at risk for uncontrolled hypertension or protects them from it.
We found that the low socio-economic status of the slum residents, coupled with high medication prices, limited treatment.
Gaps in care persist in urban areas
Nairobi’s slum dwellers experience sub-optimal access to essential services. They face conditions that make informal settlements vulnerable to emergencies such as disease outbreaks and natural disasters.
Even though there are effective treatments for hypertension, gaps in care persist in urban areas in Kenya, particularly among the poorest communities.
Our research aimed at understanding the barriers to blood pressure control at various levels—individual, family and community, health system and policy.
We collected data through interviews and focus groups in two Nairobi slums: Korogocho and Viwandani. We interviewed people who had uncontrolled hypertension, aiming to understand their experiences and perspectives about their care.
Health care providers were interviewed to gather information about their prescription practices, adherence to national guidelines and knowledge of hypertension.
We also interviewed decision-makers and policymakers to gain their views on the challenges faced in getting hypertension care in the study community.
The research identified barriers to blood pressure control across all the levels studied. Major bottlenecks were the high cost of hypertension medicines, the constant unavailability of medicines at health facilities, and an unsupportive family and environment.
In this study, access to medication was a major barrier to blood pressure control.
Countries such as Eritrea and South Africa provide free hypertension medications at the community level.
In Kenya, however, free medication is provided only at higher-level health facilities. Slum residents have access to lower-level facilities which are not mandated to provide hypertension medications.
So what can be done?
A viable approach is to implement programs with interventions capable of addressing the complex array of factors influencing hypertension care.
For instance, the provision of free or subsidized medicines would remove barriers that hinder patients’ access to hypertension medication.
It’s also essential to implement policies and directives to ensure equitable care for all, including those in slum communities seeking care at lower-level health facilities.
Provided by
The Conversation
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Source: Read Full Article
