Autistic individuals often rely on Medicaid for insurance, but the transition to adulthood can, and often does, impact their enrollment status. In continuing to examine how autistic individuals use Medicaid, recent research from Drexel University’s A.J. Drexel Autism Institute has identified a trend in intellectual disability diagnoses among autistic young people that is likely indicative of a system-wide problem that makes it difficult for them to maintain coverage into adulthood.
It’s estimated that one in three autistic people use Medicaid, with nearly 70% of the enrollees being children. During the transition to adulthood, autistic young adults’ coverage can be disrupted for many reasons. At age 19, autistic young adults are reassessed for Medicaid eligibility as an individual—rather than being allowed to continue coverage as part of their family.
At age 21 most states terminate autism support resources provided by the education system, which can also disrupt Medicaid access. And most states don’t have autism-specific eligibility criteria included in their Medicaid waivers, and most states that do have autism-specific eligibility criteria only cover children. This means people whose only medical diagnosis is autism may not be eligible to continue Medicaid coverage as an adult.
Medicaid’s waiver system is currently set up to allow tailored health care services for individuals diagnosed with an intellectual disability through their transition to adulthood. Intellectual and developmental disabilities are a larger class of conditions, including autism, which is characterized by its social-behavioral differences and repetitive or restricted behaviors.
The Centers for Disease Control and Prevention (CDC) uses the term intellectual disability when there are limits to a person’s ability to learn and function in daily life. For the vast majority of individuals diagnosed with autism or intellectual disability, those diagnoses are made in childhood—typically by age 8.
Previous research has found that during the transition to adulthood, autistic individuals are more likely than their non-autistic peers with intellectual disability to lose their Medicaid benefits and not re-enroll. To examine this more closely, the Drexel team decided to look at whether autistic young people who experienced disenrollment from Medicaid were actually more likely than autistic young people who had not experienced disenrollment to be diagnosed with intellectual disability in adulthood.
Led by Meghan Carey, a doctoral student in the Epidemiology and Biostatistics department in the Dornsife School of Public Health, the research team examined national Medicaid claims data from the 2008–2016 to study the probability of autistic young people, who did not have an intellectual disability diagnosis in their first year of Medicaid enrollment, receiving an intellectual disability diagnosis later.
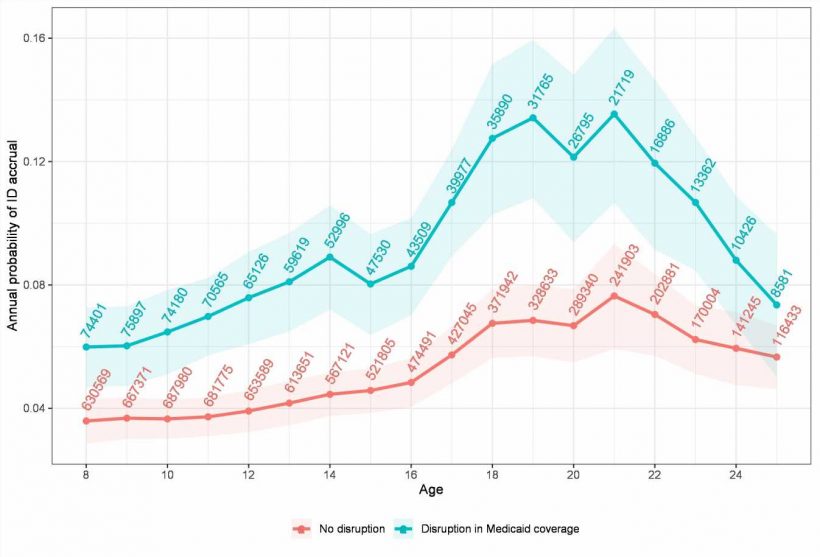
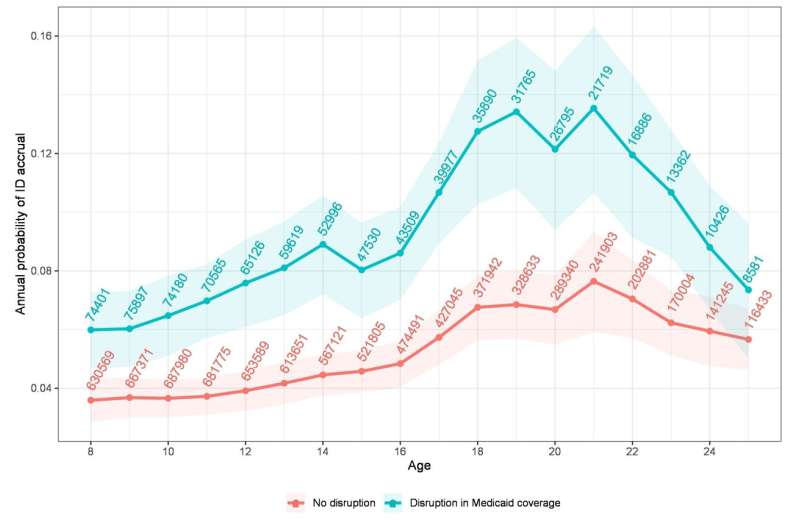
“We found that one in five autistic individuals, ages 8-25, received an intellectual disability diagnosis during follow-up,” said Carey. She also noted that while the co-occurrence of intellectual disability among the autistic population enrolled in Medicaid is common—about 25%—intellectual disability is most often diagnosable in early childhood, especially as children enter school when cognitive testing is delivered more frequently.
“We would expect the number of accrued intellectual disability diagnoses after age 8 to be substantially lower than the observed 19%,” said Carey. “Further, the American Psychological Association suggests any newly acquired intellectual disability after age 18 should be diagnosed as a neurocognitive disorder or another diagnosis, unless there was a traumatic brain injury, which is inconsistent with the peaks of intellectual disability accrual at ages 19 and 21 observed in this study.”
Because most states don’t have autism-specific criteria for Medicaid eligibility, Carey noted the research team hypothesized, and found, that autistic individuals who experience disruptions in Medicaid coverage—or periods of disenrollment—would be more likely accrue an intellectual disability diagnosis later, because in their home state, their autism diagnosis alone was potentially insufficient for retaining Medicaid coverage.
“New intellectual disability diagnoses may help autistic youth with coverage disruptions regain—or when receiving a diagnosis proactively, retain—Medicaid coverage and allow for continued health care service access,” said Carey. “However, it may also mean that autistic young people are no longer receiving services related to their autism diagnosis, which could have negative effects on their health.”
Carey and her co-authors hope that this research strengthens the call to ensure lifelong Medicaid coverage for autistic people.
One solution to this problem, the team suggests, would be to adjust Medicaid waivers. A change to states’ waivers that ensures adequate coverage for autistic people without a co-occurring intellectual disability diagnosis, and ensures continuity in coverage through adulthood, could be an effective approach to mitigate these disruptions to Medicaid coverage—and the need for people to be reexamined for intellectual disability diagnoses in young adulthood, according to the research team.
“Their service needs don’t just end when they become adults,” said Carey. “Given Medicaid is a critical safety net insurer and the lifelong needs of autistic individuals, policies aimed at ensuring Medicaid coverage continues from childhood throughout adulthood are essential to meet the health care-related needs for autistic people.”
The findings are published in the journal Autism.
More information:
Meghan E Carey et al, Short report on navigating access to care for Medicaid-enrolled autistic youth and young adults: Examining accrual of intellectual disability diagnoses in adolescence, Autism (2023). DOI: 10.1177/13623613231177559
Journal information:
Autism
Source: Read Full Article