A recent study published in the journal Respiratory Research found impaired lung function and dyspnea amongst severe COVID-19 pneumonia survivors one year post-infection. Meanwhile, many COVID-19 patients developed fibrotic-like sequelae as an aftermath of the infection-associated mild or severe pneumonia.
 Study: Lung function and radiological findings 1 year after COVID-19: a prospective follow-up. Image Credit: People Image Studio / Shutterstock
Study: Lung function and radiological findings 1 year after COVID-19: a prospective follow-up. Image Credit: People Image Studio / Shutterstock
Background
First reported in Wuhan, China, at the end of 2019, the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) outbreak has spread globally to cause the coronavirus disease 2019 (COVID-19), which has claimed the lives of more than 6.5 million people worldwide. The disease mainly infects the respiratory system and precipitates long-term sequelae often referred to as post-COVID syndrome or long COVID.
Symptoms of long COVID range from lingering headaches and myalgia to permanent disabilities, affecting the survivors' quality of life. Nearly one-third of the infected patients develop acute respiratory distress syndrome (ARDS), while fibrotic pulmonary lesions develop in many.
Evidence suggests that patients on mechanical ventilation during the acute phase of COVID-19 sustain more alterations in their pneumocytes, pulmonary endothelial and alveolar cells, as well as interstitial and pulmonary fibrotic changes compared to those on conventional oxygen. One-fourth of the patients who developed pneumonia suffered from sub-pleural cystic/reticular lesions, and one-third of the patients had fibrotic changes following one year and six months post-discharge, respectively.
The study
This multicenter, prospective, observational cohort study evaluated patients with bilateral pneumonia as a pulmonary sequela of SARS-CoV-2 infection – for lung function alterations and persistent fibrous lesions one year after hospital discharge.
The study was conducted in Spain and enrolled all adult patients discharged from respiratory services with a life expectancy of more than one year. Functional changes, the evolution of dyspnea, and exercise capacity were evaluated after discharge––at two months (V1), six months (V2), and twelve months (V3).
Results of the study
The mean age of the participants was 60.5 years, and the majority were males. Notably, males showed a greater preponderance of more severe disease. In addition, the duration of hospital stay, the laboratory parameters (C-reactive protein, lymphocyte count, lactate dehydrogenase levels, D-dimer, and ferritin), and RALE scores varied between the study groups (vis, V1, V2, and V3). Whereas there were no significant differences amongst the study groups concerning patients' demographics, such as – body mass index (BMI), age, smoking, and comorbidities.
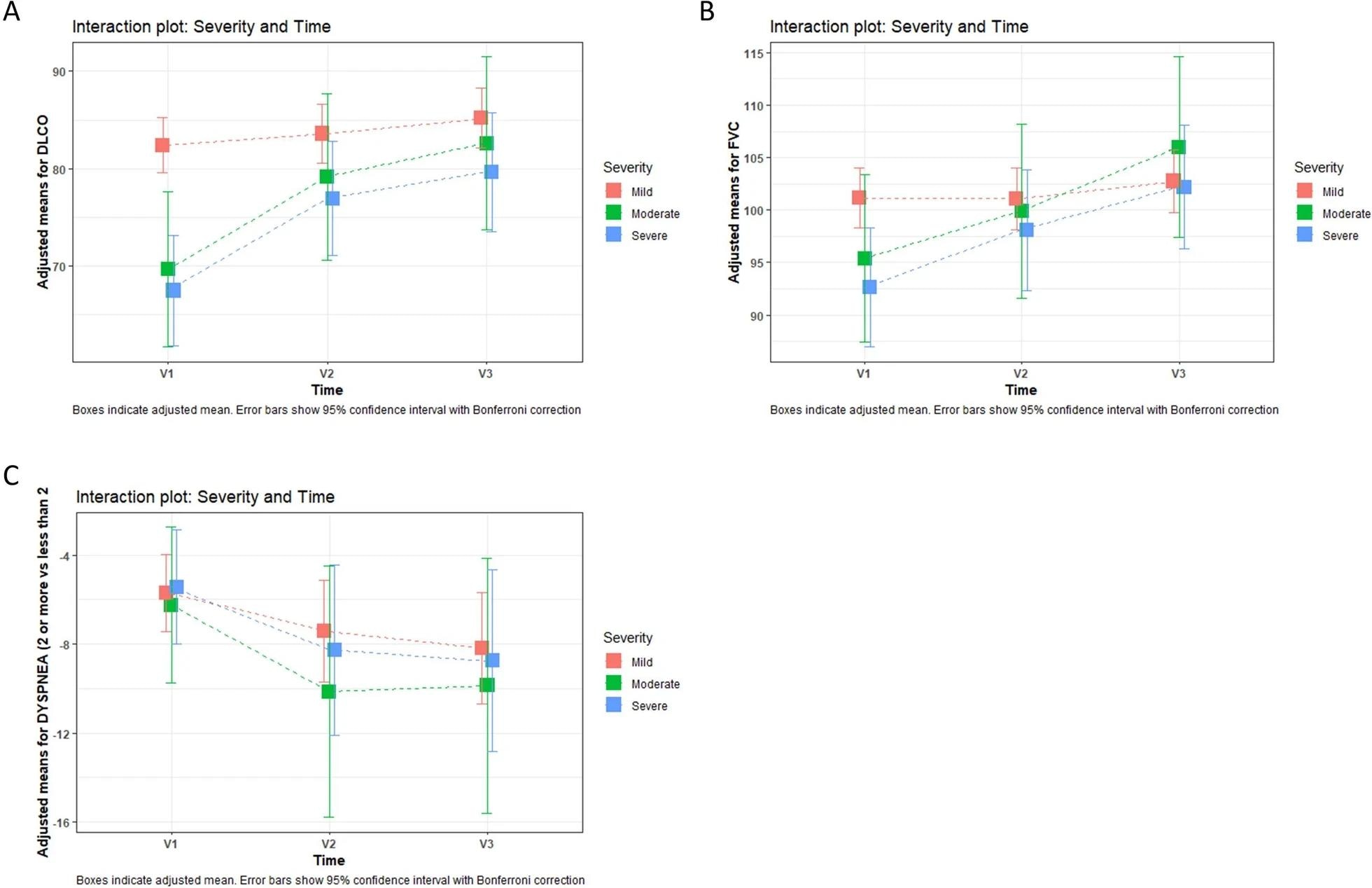
Interaction plot of severity and time based on linear mixed model post-hoc analysis. Boxes indicate adjusted mean. Error bars show 95% confidence interval with Bonferroni correction. V1 (2 months), V2 (6 months) and V3 (12 months). Group 1: mild; group 2: moderate; group 3: severe. A Interaction plot: changes over time and severity in % of predicted DLCO. We found differences between mind and moderate [p = 0.001] or severe [p < 0.001] patients only at 2 months (V1). B Interaction plot: changes over time and severity in FVC% of predicted. No between-group differences were found at any time. C Interaction plot: changes over time and severity in dyspnea. No between-group differences were found at any time. FVC forced vital capacity, DLCO diffusing capacity of lungs for carbon monoxide.
Pulmonary function tests revealed that 53.8% of patients had impaired diffusion after two months, which gradually improved after six months and one year. The mean diffusing capacity of the lungs for carbon monoxide (DLCO) abnormalities was 78.5 in V1, 81.6 in V2, and 84 in V3. Significant alterations in diffusion were found at 60 days––relative to time and severity––between mild, moderate, and severe patients.
Throughout the cohort, a restricted abnormality was seen in 14.3% of patients at two months, 9.3% at six months, and 6.7% at 12 months. The mean forced vital capacity (FVC) was 99 at V1, 100.8 at V2, and 104.2 at V3. Meanwhile, no significant differences were found in FVC relative to time and severity.
Next, the cohort was analyzed for dyspnea. The mMRC scale depicted dyspnea ≥ 2 in 21.5% of the patients at V1, 11.3% at V2, and 9.8% at V3. A significant association was found between dyspnea and the time of follow-up. However, time-dependent significant differences among the severity groups were absent.
In addition, lung static volumes remained comparable between the groups, while the six-minute walk test (6MWT) showed differences in the distance walked – with severity as the confounding factor. Altered DLCO (of <80% at 12 months) is associated with age, female gender, ferritin levels, and BMI.
Computed tomography (CT) was advised two months post-discharge in patients with abnormal chest X-rays, abnormal pulmonary function test results, and persistent dyspnea. HRCT was performed after two months on 325 patients. Among these, 38.4% revealed complete resolution, while the remaining exhibited ground glass opacities (GGO). Notably, GGO was the most common (in 73.5%) and showed differences based on age groups.
CT was repeated in patients with prior abnormal CT findings one-year post-discharge. Overall, 156 out of 200 patients had CT at V3 – 78.8 % of whom showed persistent radiological alterations. Of the 200 patients, 45.5% had GGO; the reticular pattern was found in 34% of patients; parenchymal bands were found in 33.4%, and traction bronchiectasis was seen in 30.8%.
Out of 156 patients, 102 revealed fibrotic-like sequelae – depicted by CT conducted at 12 months. Significant changes between age groups were more frequently detected in severe cases.
Lactate dehydrogenase (LDH) and the involvement of the lungs, as seen in radiology during admission, were associated with the fibrotic pattern at V3.
Conclusion
Many patients with pneumonia associated with SARS-CoV-2 infection developed fibrous sequelae and showed dyspnea and impairments in lung function one year after hospital discharge. Therefore, further follow-ups of the patients who suffered from severe COVID-19-associated pneumonia are warranted to study the progression of the fibrotic lesions over time.
- Tarraso, J., Safont, B., Carbonell-Asins, J., et al. (2022). Lung function and radiological findings 1 year after COVID-19: a prospective follow-up. Respiratory Research. Doi: 10.1186/s12931-022-02166-8, https://respiratory-research.biomedcentral.com/articles/10.1186/s12931-022-02166-8
Posted in: Men's Health News | Medical Research News | Medical Condition News | Women's Health News | Disease/Infection News
Tags: Acute Respiratory Distress Syndrome, Body Mass Index, Bronchiectasis, Carbon Monoxide, Computed Tomography, Coronavirus, Coronavirus Disease COVID-19, covid-19, C-Reactive Protein, CT, D-dimer, Dyspnea, Evolution, Exercise, Hospital, Laboratory, Life Expectancy, Lungs, Lymphocyte, Oxygen, Pneumonia, Protein, Radiology, Research, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Smoking, Syndrome, Tomography, Traction

Written by
Nidhi Saha
I am a medical content writer and editor. My interests lie in public health awareness and medical communication. I have worked as a clinical dentist and as a consultant research writer in an Indian medical publishing house. It is my constant endeavor is to update knowledge on newer treatment modalities relating to various medical fields. I have also aided in proofreading and publication of manuscripts in accredited medical journals. I like to sketch, read and listen to music in my leisure time.
Source: Read Full Article
