Phototherapy is a safe, effective, noninvasive, and inexpensive way of boosting cognition for patients with dementia, new research suggests. It may be “one of the most promising interventions for improving core symptoms” of the disease.
A new meta-analysis shows that patients with dementia who received phototherapy experienced significant cognitive improvement, compared to those who received usual treatment. However, there were no differences between study groups in terms of improved depression, agitation, or sleep problems.
“Our meta-analysis indicates that phototherapy improved cognitive function in patients with dementia…. This suggests that phototherapy may be one of the most promising non-pharmacological interventions for improving core symptoms of dementia,” the investigators, led by Xinlian Lu, School of Psychological and Cognitive Sciences, Peking University, Beijing, China, write.
The study was published online April 5 in Brain and Behavior.
A New Treatment Option?
“As drug treatment for dementia has limitations such as medical contraindications, limited efficacy, and adverse effects, non-pharmacological therapy has been increasingly regarded as a critical part of comprehensive dementia care,” the investigators note.
Phototherapy, which utilizes full-spectrum bright light (usually >600 lux) or wavelength-specific light (eg, blue-enriched or blue-green), is a “promising non-pharmacological therapy” that is noninvasive, inexpensive, and safe.
Most studies of phototherapy have focused on sleep. Findings have shown “high heterogeneity” among the interventions and the populations in the studies, and results have been “inconsistent.” In addition, the effect of phototherapy on cognitive function and behavioral and psychological symptoms of dementia (BPSD) “still need to be clarified.”
In the systematic review and meta-analysis, investigators examined the effects of phototherapy on cognitive function, BPSD, and sleep in older adults with dementia.
They searched several databases for randomized controlled trials that investigated phototherapy interventions for elderly patients. The primary outcome was cognitive function, which was assessed via the Mini-Mental State Examination (MMSE).
Secondary outcomes included BPSD, including agitation, anxiety, irritability, depression, anxiety, and sleep disturbances, as assessed by the Cornell Scale for Depression in Dementia (CSDD), the Cohen-Mansfield Agitation Inventory (CMAI), the Neuropsychiatric Inventory (NPI), and measures of sleep, including total sleep time (TST), sleep efficiency (SE), and sleep disorders, as assessed by the Sleep Disorder Inventory (SDI).
To be included in the analysis, individual studies had to focus on elderly adults who had some form of dementia. In addition, a group receiving a phototherapy intervention had to be compared to a nonintervention group, and the study had to specify one of the above-defined outcomes.
The review included phototherapy interventions of all forms, frequencies, and durations, including use of bright light, LED light, and blue or blue-green light.
Regulating Circadian Rhythm
Twelve studies met the researchers’ criteria. They included a total of 766 patients with dementia ― 426 in the intervention group and 340 in the control group. The mean ages ranged from 73.73 to 85.9 years, and there was a greater number of female than male participants.
Of the studies, seven employed routine daily light in the control group, while the others used either dim light (≤50 lux) or devices without light.
The researchers found “significant positive intervention effects” for global cognitive function. Improvements in postintervention MMSE scores differed significantly between the experimental groups and control groups (mean difference [MD], 2.68; 95% CI, 1.38 – 3.98; I2 = 0%).
No significant differences were found in the effects of intervention on depression symptoms, as evidenced in CSDD scores (MD, −0.70; 95% CI, −3.10 to 1.70; I2 = 81%).
Among patients with higher CMAI scores, which indicate more severe agitation behaviors, there was a “trend of decreasing CMAI scores” after phototherapy (MD, −3.12; 95% CI, −8.05 to 1.82; I2 = 0%). No significant difference in NPI scores was observed between the two groups.
Similarly, no significant difference was found between the two groups in TST, SE, or SDI scores.
Adverse effects were infrequent and were not severe. Two of the 426 patients in the intervention group experienced mild ocular irritation, and one experienced slight transient redness of the forehead.
Light “may compensate for the reduction in the visual sensory input of patients with dementia and stimulate specific neurons in the suprachiasmatic nucleus of the hypothalamus to regulate circadian rhythm,” the researchers suggest.
“As circadian rhythms are involved in optimal brain function, light supplementation may act on the synchronizing/phase-shifting effects of circadian rhythms to improve cognitive function,” they add.
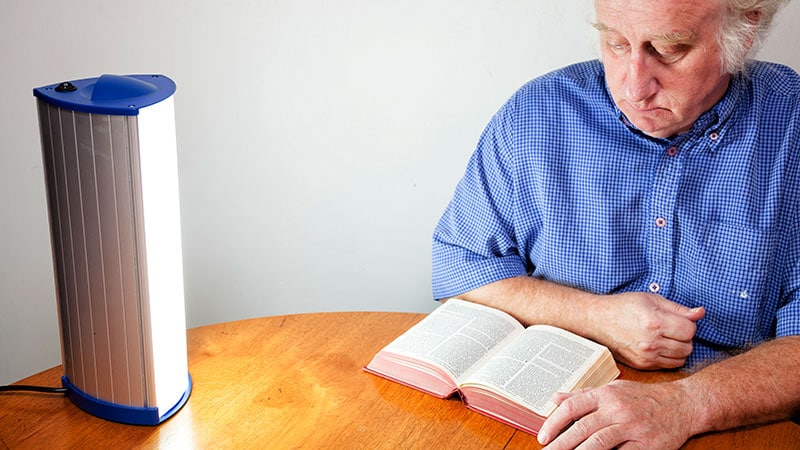
They note that the light box is the “most commonly used device in phototherapy.” Light boxes provide full-spectrum bright light, usually >2500 lux. The duration is 30 minutes in the daytime, and treatment lasts 4 to 8 weeks.
The investigators caution that the light box should be placed 60 cm away from the patient or above the patient’s eye level. They say that a ceiling-mounted light is a “good choice” for providing whole-day phototherapy, since such lights do not interfere with the patient’s daily routine, reduce the demand on staff, and contribute to better adherence.
Phototherapy helmets and glasses are also available. These portable devices “allow for better control of light intensity and are ergonomic without interfering with patients’ normal activities.”
The researchers note that “further well-designed studies are needed to explore the most effective clinical implementation conditions, including device type, duration, frequency, and time.”
Easy to Use
Commenting for Medscape Medical News, Mariana Figueiro, PhD, professor and director of the Light and Health Research Center, Department of Population Health Medicine, Icahn School of Medicine at Mount Sinai, New York, said light is the “major stimulus for the circadian system, and a robust light-dark pattern daily (which can be given by light therapy during the day) improves sleep and behavior and reduces depression and agitation.”
Figueiro, who was not involved with the current study, noted that patients with dementia “have sleep issues, which can further affect their cognition; improvement in sleep leads to improvement in cognition,” and this may be an underlying mechanism associated with these results.
The clinical significance of the study “is that this is a nonpharmacological intervention and can be easily applied in the homes or controlled facilities, and it can be used with any other medication,” she pointed out.
“More importantly, sleep medications have negative side effects, so the use of nonpharmacological interventions improving sleep and cognition is great for clinical practice,” she added.
However, she took issue with the finding that phototherapy was not effective for depression and agitation, noting that there were “too few studies to say for sure that light therapy is ineffective at improving these outcomes.”
The research received no external funding. The authors and Figueiro hae disclosed no relevant financial relationships.
Brain Behav. Published online April 5, 2023. Full text
Batya Swift Yasgur, MA, LSW is a freelance writer with a counseling practice in Teaneck, New Jersey. She is a regular contributor to numerous medical publications, including Medscape and WebMD, and is the author of several consumer-oriented health books as well as Behind the Burqa: Our Lives in Afghanistan and How We Escaped to Freedom(the memoir of two brave Afghan sisters who told her their story).
For more news, follow Medscape on Facebook, Twitter, Instagram, and YouTube.
Source: Read Full Article