Scientists from Duke-NUS Medical School and their collaborators have come up with new methods to cultivate brain cells from stem cells to treat and study neurodegenerative diseases. This novel technology forms the basis of two recent research projects under the newly established GK Goh Center for Neuroscience (the GK Goh Center) at Duke-NUS, offering hope for new treatments to patients suffering from neurological conditions such as Alzheimer’s disease, ischemic stroke and Parkinson’s Disease.
The GK Goh Center was established within Duke-NUS’ Neuroscience & Behavioral Disorders (NBD) Program to investigate the impact of aging on the brain through findings such as these. It is led by neuroscientist Professor Zhang Suchun, who is also the director of Duke-NUS’ NBD Program.
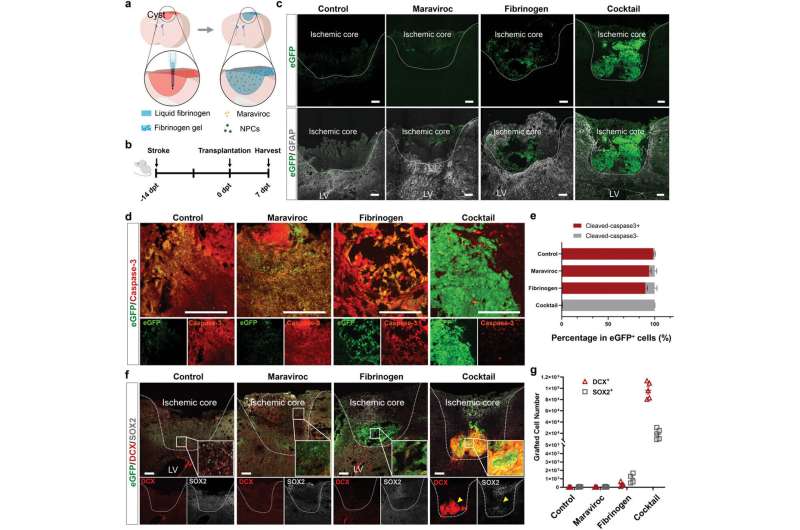
In the first research project, which was published in Advanced Science, scientists successfully grew neurons (nerve cells) from stem cells for transplantation into stroke patients to repair damaged brain tissue.
The cells were cultivated on a chemical cocktail made up of Fibrinogen, a protein that helps with blood clotting; and Maraviroc, a drug used to treat infection. This mixture protected the cells from inflammation when they were transplanted into the highly inflamed environment of a brain affected by ischemic stroke.
In preclinical trials, the cells not only survived, but successfully matured into the target neuron type and repaired the damaged brain over a period of 30 days. Prior to this discovery, transplanted cells had poor survival rates as most of them would die in the ischemic cavity of the brain due to inflammation.
Ischemic stroke, which occurs when blood supply to the brain is suddenly reduced, is a leading cause of death and disability worldwide. Globally, one in four people over the age of 25 will have a stroke in their lifetime. To date, the only opportunity to mitigate the damage caused by stroke lies within the first six hours after the event. Even then, almost all survivors do not recover fully, living with disabilities, such as paralysis and cognitive impairment. No treatments are available that can fully restore function.
“The human brain has a very limited capacity to regenerate so there is a need for more effective treatment for neurological diseases. Stem cell-based approaches hold promise as they can protect the injured neurons from further damage and replace lost neurons. Our transplantation method has proven that cultivated cells can mature to become functional neurons and potentially integrate into brain circuitry in conditions such as stroke, spinal cord injury and Parkinson’s disease,” said Dr. Wang Zhifu, lead author of the study, and a research fellow with Duke-NUS’ NBD Program.
The team has licensed the method and patent applications are underway for this technology, which has also proven successful in other neurodegenerative diseases, including Parkinson’s disease. In previous studies of Parkinson’s disease, Prof Zhang and his collaborators have used their method to produce dopamine neurons. These cells, which are located in the midbrain, degenerate with the onset of the disease.
The healthy neurons that were cultivated can then be transplanted into the brains of those with Parkinson’s disease, where the cells grow and regenerate damaged tissue in the process. The research findings were published in Cell Stem Cell and Nature Medicine. The team is seeking approval from US regulators to start human safety clinical trials.
“While its inaccessibility makes any study of the brain challenging, our strategy is to use the new technology to guide stem cells to develop into various types of neurons. With these functional brain cells, we can study how they age and uncover their roles in neurodegenerative conditions. The new insights will help in finding new and more effective therapies to treat brain diseases and perhaps even slow down the aging process,” said Prof Zhang.
Using the same technology, the team at the GK Goh Center is also the first in the world to produce norepinephrine neurons—specialized nerve cells located in the brainstem, which connects with every part of the brain and spinal cord. These neurons degenerate in many conditions such as Alzheimer’s disease and Parkinson’s disease—often as early as 10 years before symptom onset. The production of these cells will enable scientists to study why they are vulnerable and how their degeneration causes the diseases. This research was published in Nature Biotechnology.
“I am delighted that our scientists have already made impactful findings that will go a long way to help patients suffering from neurodegenerative diseases in Singapore. I am confident that this Center will continue to enable Duke-NUS to deliver innovative bedside interventions that will not only improve the quality of life for the individual but also support our nation’s efforts on healthier aging,” said Mr. GK Goh, who is also Chairman Emeritus of the international executive board of Temasek Foundation International and a member of the board of Temasek Foundation.
“The potential for this novel technology is limitless. Professor Zhang and his team have cultivated more than a dozen different types of functioning neurons, including those in the brain, eye and spinal cord,” said Professor Thomas Coffman, Dean, Duke-NUS.
“They have also collected a vast spectrum of biological samples that they can use in tandem to decode how the brain ages, a physiological process we still know little about. We are thankful for the donation by the G.K. Goh family, which will offer us the means to test drugs and develop new therapies for otherwise incurable brain conditions.”
More information:
Zhifu Wang et al, Enabling Survival of Transplanted Neural Precursor Cells in the Ischemic Brain, Advanced Science (2023). DOI: 10.1002/advs.202302527
Yunlong Tao et al, Generation of locus coeruleus norepinephrine neurons from human pluripotent stem cells, Nature Biotechnology (2023). DOI: 10.1038/s41587-023-01977-4
Source: Read Full Article
