One in every 1,000 patients with epilepsy dies suddenly every year. Researchers have confirmed that some severe-type seizures (generalized convulsive seizures—GCS) are the most consistent risk factor for Sudden Unexpected Death in Epilepsy (SUDEP). In the past few years, heart rate variability (HRV) has been studied as a potential biomarker to identify patients at greater risk of SUDEP, in whom specific interventions could be made to prevent sudden death. A multidisciplinary team of researchers from Centro Hospitalar Universitário de São João and INESC TEC—Institute for Systems and Computer Engineering, Technology and Science, in Portugal, have been conducting studies on this topic.
Imagine you are seating in your living room, with your family or friends, watching your favorite Netflix show. Suddenly, you seem to lose conscience. All the muscles in your body start to tighten and your body quickly stiffens as a wood plank. You fall to the ground because you can no longer sit. Everyone starts to wonder what is happening with you, worried. Soon after, your limbs jerk around uncontrollably. Eventually, you regain conscience and have no recollection of what happened. This is what an epilepsy seizure can look like.
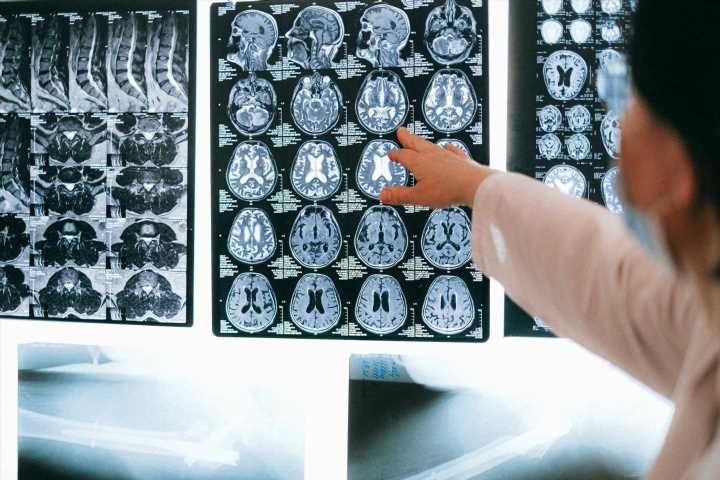
What is epilepsy?
Epilepsy is a common neurological condition that affects the brain, usually known for the seizures it causes. According to the World Health Organization (WHO), around 50 million people in the world suffer from epilepsy, most of those living in low and middle-income countries. If some epilepsy patients can reduce the number and severity of seizures through medication, others don’t seem to improve over the years. The latter are usually diagnosed with refractory or drug-resistant epilepsy. Because the medication is not effective, these refractory epilepsy patients are the ones whose seizures are more frequent and severe.
There are many types of epileptic seizures. As stated by the Epilepsy Foundation, seizures can be categorized according to the extent to which the brain is affected. Those that affect one area in one side of the brain are called ‘Focal onset seizures’ as opposed to ‘Generalized onset seizures’ that typically affect both sides of the brain simultaneously. But even focal seizures can generalize secondarily. We call generalized convulsive seizures (GCS) those that generalize, independently of having a focal or generalized onset. These are the category of seizures the Portuguese researchers have delved into.
The most severe epileptic seizures
The first study of the Portuguese team entitled “Heart rate variability in patients with refractory epilepsy: The influence of generalized convulsive seizures” focused on GCS. These are characterized by stiffing of all the muscles in the body (tonic) and the rapid movement of arms and legs (clonic). The team studied cardiac changes in patients with refractory epilepsy, later comparing the results with the general population.
“We evaluated 121 patients and measured Heart Rate Variability (HRV) parameters of these patients before and after having a seizure. The patients with refractory epilepsy had a significant reduction in HRV parameters when compared with a normative healthy population,” said Maria Teresa Faria, Head of the Nuclear Medicine Department of the Centro Hospitalar Universitário de São João.
HRV is the measure of time between each heartbeat. Unlike a metronome, if a human heart beats 60 times per minute, it doesn’t mean it beats exactly every second. This variation is considered good because it means your heart can respond to the autonomic nervous system, being ready for either increasing or decreasing the heart rate as necessary.
As GCS is one of the most severe types of seizures, the researchers wanted to confirm with another study (“Does the type of seizure influence heart rate variability changes?”) that these seizures affect the HRV parameters more than other types of seizures and, consequently, could mean an increased risk of SUDEP. “The studies that compare alterations of GCS and non-GCS are limited, and most of those do not compare the same patients, as we did. The autonomic response varies from one patient to another, which is why we studied only patients who presented both types of seizures,” claimed the doctor. As anticipated, the results have indicated that GCS, compared with other types of seizures, have a greater effect on autonomic cardiac function, which may be associated with an increased risk of SUDEP.
Higher risk of sudden death
If GCS can lower HRV parameters, and knowing that a low HRV is associated with a greater risk of sudden death in many other diseases, then monitoring HRV could be a way to identify which patients with epilepsy are at greater risk of SUDEP. “The monitoring of HRV has not been included by neurologists as a follow-up procedure yet, but patients with more HRV changes may have a greater risk of SUDEP,” added Maria Teresa Faria.
The research work has gone a long way into assessing these patients; however, there is still a lot of data to crunch. “We have data that allows us to monitor HRV and specific cardiac analytic serum biomarkers. We will be able to verify if changes in a parameter depend on another or not, thus allowing us to understand if SUDEP has a multifactorial cause or not,” stated Maria Teresa Faria.
The data analysis is a key factor for detecting changes in HRV parameters, and this was done by the INESC TEC engineers. “We have developed advanced systems and algorithms for HRV analysis (some patented) that we applied in this cooperation with Centro Hospitalar Universitário de São João. With this technology, we could support quantitatively the MD’s hypothesis that GCS induce lower HRV parameters, and thus lower vagus tone, which has been associated with a higher risk of sudden death,” said Susana Rodrigues, co-author and researcher at INESC TEC.
Source: Read Full Article