The genetic code of the new coronavirus has been found: it is closely related to the SARS virus from 2003. Professor of Molecular Virology, Eric Snijder, has been researching coronaviruses for years. We asked him a few questions about the outbreak.
We learned this week that the official name of the virus is SARS-CoV-2, and had already heard that it is closely related to the SARS virus from 2003. What does that mean?
The two viruses are genetically related: around 80% of their genome is identical. According to the official virus taxonomy, the two belong to the same virus species. This genetic relationship does not necessarily mean that they cause the same infections, however. Sometimes there are viruses within a single species that infect different hosts: within alpha-coronavirus-1 there is a dog coronavirus, a cat virus and a virus that infects pigs.
Is this virus as dangerous as the SARS virus from 2003? Or is it more dangerous still?
We don’t really know yet, also because the outbreak has only recently been discovered and the reliability of the figures from the Chinese government is questionable. The mortality—the number of people to die from the disease—appears to be lower: around 2% now in comparison with 10% for SARS-1, but this is obviously based on registered cases. And from the perspective of mortality, the MERS coronavirus [which occurs in the Middle East and is transmitted from dromedary camels to people, ed.] is much more dangerous: this has a mortality of 35% and has been doing the rounds for eight years already. What is also important to the risk assessment is how easily the virus can be transmitted from one person to another. In virology we call the level of contagion the R0, the basic reproduction number. This appears to be higher for this new virus than for SARS-1. The R0 for MERS is very low in contrast.
How long before there is a vaccine for this virus?
It’s really hard to say, but it certainly won’t be soon. We may have the prototype of a vaccine within a few months—that’s when the first animal tests will have been completed—but the most important part is still to come: is the vaccine both safe and effective in humans? A coronavirus vaccine for humans has never been developed and tested before, so we have no experience whatsoever with it. Then the larger-scale clinical trials follow, unless the decision is made to bypass them completely because of the urgency of the situation, and then you have to scale up the production of the vaccine until a potential several hundred million doses. If you compare that with our annual flu jab, we now have a streamlined procedure and know the virus through and through, but even then the production time is still nine months.
We already knew SARS-1, MERS in the Middle East and now this new variant: what is it about coronaviruses that make them so good at causing global epidemics?
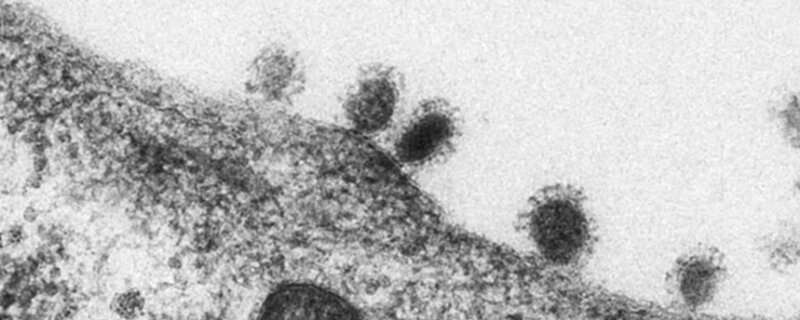
Obviously they’re not the only viruses that are capable of this, but their large genome does make them special: they have two to three times as much genetic info as most other RNA viruses. This appears to mean they have more tricks up their sleeves. They have a large number of functions that they can use to undermine the host’s virus defence, and they have a more refined way of multiplying in a host cell.
Just as in 2003, bats appear to be the source of the virus. Why are coronaviruses so good at jumping from bats to humans?
They’re both mammals, of course, so in that sense humans are similar to bats. And there are so many different bats: more than 20% of all mammal species are bats. But I think it’s also because of the SARS outbreak in 2003 that the emphasis has come to lie on bats. It was in 2005 that coronavirus was first found in bats that was reasonably closely linked to the virus outbreak in 2003. The research that followed mainly focused on this species as a possible source of the virus, when all sorts of rodents also carry coronaviruses. The tricky part is that well never be able to discover the exact source: when a virus jumps from one species to another this a one-off random process in which the virus develops exactly the right mutations to efficiently infect another host species. Unfortunately, we don’t know the parameters of this process.
What will happen when the first person is infected in the Netherlands? Are we prepared?
We are alert and prepared for a limited number of cases: everything is in place for the diagnosis, hospital admissions and tracing patient contacts. However, it’s almost impossible to protect yourself as a country—or a planet—from a really big epidemic, such as the flu. That’s why we’re focusing our efforts on keeping the epidemic small, should the first cases arise, and we’re hoping that a vaccine will be available in time.
Source: Read Full Article
