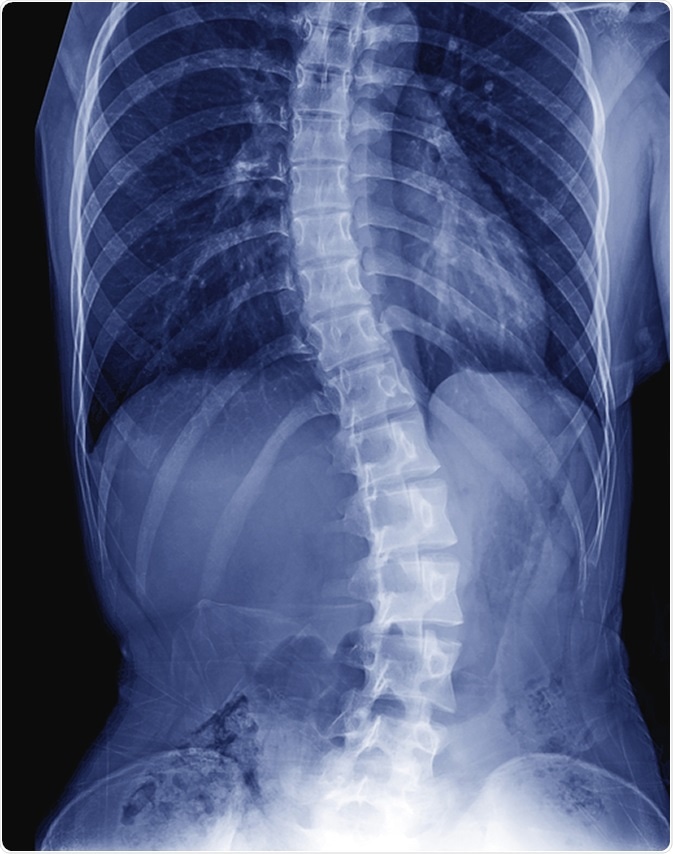
Pediatric spinal deformities are notorious for causing obvious and progressive deformities in posture, gait and appearance. Non-surgical and surgical management has been attempted over the centuries.
Nonsurgical management
The use of spinal whole body casts preceded the development of modern spinal braces, which have reduced the time required for immobilization of the spine. The material for the brace has evolved with time.
The concept behind bracing is to counteract the deforming effect of the scoliosis by the pull of opposite forces acting through the ribs or the torso. This uses normal growth forces to prevent or, at least, reduce the progression of the spinal curve. In most cases this is a holding measure but a few patients have not needed surgery following the discontinuation of the brace.
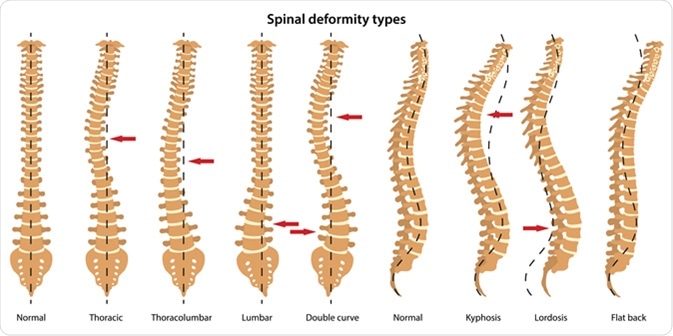
Different types of braces are used depending on the area of the spine that shows the maximum curvature, such as the thoracolumbosacral orthosis (TLSO), and the cervicothoracolumbosacral orthosis (CTLSO) like the Milwaukee brace.
The latter was meant to be worn continuously, but has now been largely replaced by modern, lighter and thermoplastic rigid TLSOs, which may be customizable.
For those who cannot tolerate day wear, nighttime bending TLSO braces are available, where overcorrection of the thoracic, lumbar or sacral spine is performed only from the evening onwards. Tension-based orthoses are also being used.
The role of bracing is under review to establish the actual success rate and the best models for general use. This depends on the actual use-time, which is best recommended to be over 12 hours a day. A very low percentage of wearers use it for more than this period in any case.
Surgical correction
The place of surgery in scoliosis is unchallenged, due to the often progressive nature of this condition and the late stage at which it is diagnosed.
Surgical correction aims at achieving a balanced spine, which is free of pain and is properly fused. It also aims to preserve maximum spine mobility, in addition to preventing cardiopulmonary difficulties. Required imaging should be done to arrive at the right degree of correction and to rule out other spinal pathologies, such as cord tethering or tumors.
The Lenke system of classification for scoliosis is the most commonly used, because it helps with selecting the right level for fusion and enables surgeons to elect to do lumbar-sparing fusions, thereby reducing secondary spinal morbidity, due to lumbar immobilization.
Spinal fusion is the backbone of spinal deformity surgery. It began without the use of instruments and depended on lengthy post-operative spinal immobilization by long body casts. This was followed by Harrington instrumentation using two points of fusion above and below the curve, but still needed a prolonged period of immobilization. Segmental fixation is the present standard of care, using hooks and wires at multiple points.
The current management depends upon pedicle screw fixation, which can correct the curve more powerfully and fuses shorter segments of the spine, thus allowing a greater final spinal length. No bracing or rest is required after the procedure, which is a great advantage. The success of the technique depends on the formation of a firm bony union over time, which should precede the time of normal implant fatigue.
Normal activity is usually possible within 6-12 months after the surgery. Other procedures used in hemi-vertebra include excision of the hemi-vertebra, using an anterior-posterior or wholly posterior approach, the latter being preferred as less risky. Former techniques included hemi-epiphysiodesis, to prevent normal growth on the side of the hemi-vertebra, as well as spinal fusions and osteotomies.
Complications of surgical intervention include inadvertent interference with growth, progression of the deformity after surgery, or the occurrence of a new deformity.
Revision surgery may be needed to correct many of these, including junctional degeneration adjacent to the surgical site, undue restriction of spinal curvature or mobility, implant breakage or infection, pain due to the implant, or failure of union.
References
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3261245/
- https://www.hss.edu/conditions_revision-surgery-for-pediatric-spine-deformity.asp
- https://www.ncbi.nlm.nih.gov/pubmed/15766220
- https://www.ncbi.nlm.nih.gov/pubmed/14713581
- https://www.emoryhealthcare.org/pediatric-orthopedics/spinal-deformity.html
- http://thejns.org/doi/pdf/10.3171/foc.2003.14.1.4
- http://www.chop.edu/conditions-diseases/spinal-deformities
Further Reading
- All Scoliosis Content
- What is Scoliosis?
- Scoliosis Symptoms
- Scoliosis Cause
- Scoliosis Investigation
Last Updated: Jan 29, 2019

Written by
Dr. Liji Thomas
Dr. Liji Thomas is an OB-GYN, who graduated from the Government Medical College, University of Calicut, Kerala, in 2001. Liji practiced as a full-time consultant in obstetrics/gynecology in a private hospital for a few years following her graduation. She has counseled hundreds of patients facing issues from pregnancy-related problems and infertility, and has been in charge of over 2,000 deliveries, striving always to achieve a normal delivery rather than operative.
Source: Read Full Article
