Cervical cancer rates in Britain halved between the late 1980s and mid-2000s but progress has since been “stalling and stagnating,” according to Cancer Research UK figures published today during cervical cancer prevention week.
Thanks to research developing tests and tools that can prevent the deadly disease, such as the national screening program introduced in 1988, thousands of cervical cancers have been prevented. But the latest data marks a decade-long lack of progress, including a steep (54 percent) rise in rates among 25- to 29-year-olds, and suggests these potentially life-saving interventions don’t always reach the people who need them.
Latest figures show less than three-quarters of women invited for cervical screening take it up—and this falls even further in younger age groups and more deprived regions. Cancer Research UK believes this is part of the reason why cervical cancer still affects over 3,000 people each year.
32-year-old Gem Sofianos from London is an advocate for cervical screening since it led to her cancer diagnosis in 2015. She said: “I was young and healthy and hadn’t experienced any symptoms, so to be told I had cervical cancer took me completely by surprise. My mum accompanied me to the appointment and we just stared at each other in shocked silence. It was a lot to take in.”
Gem’s cancer was discovered early (stage 1B) and she had surgery a month later. Treatment was successful but she still has regular screening to check the cancer hasn’t come back. Gem explained: “The test takes just minutes and can save lives; I believe it saved mine. Had I left it a few more months, I might be facing a completely different battle with a very different outcome.”
Cancer Research UK is working to unpick why people don’t go for cervical screening, identifying the barriers so they can be removed. Research carried out by the charity found that around four in 10 who didn’t attend put it down to embarrassment, while two in 10 were worried it might hurt. Others said they had no symptoms to get checked out or just didn’t feel they were at risk, revealing a lack of awareness about how screening works and who it’s for.
Cervical cancer incidence rates in Britain show a clear spike in 2009, when more people attended screening and were subsequently diagnosed. Cervical screening attendance in March that year was 70 percent higher than usual following TV star Jade Goody’s untimely and tragic diagnosis, highlighting the impact that greater awareness can have.
As well as working to improve cervical screening attendance, research is ongoing into new methods like urine tests and home testing kits, which could help to overcome the practical and emotional barriers that some people face with the current program.
Cancer Research UK’s chief executive Michelle Mitchell said: “These figures show how research has protected thousands of people in the UK from cervical cancer, but they also highlight a worrying trend that shows progress is stalling and stagnating, which could undermine this success.
“Cervical cancer is one of the few cancers that can be prevented through screening, and now the disease is far less common in the UK. But these life-saving programs can’t help people they can’t reach, which is why it’s important for us to continue to raise awareness and carry out research into how screening could be improved for hard-to-reach groups.”
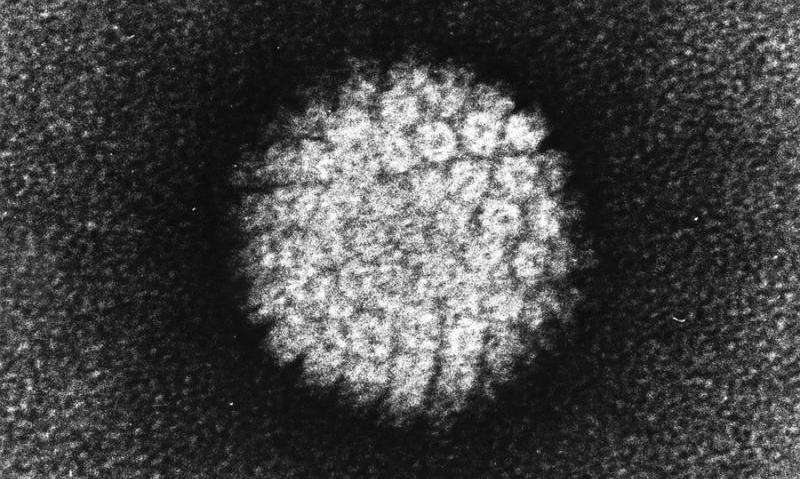
Cervical cancer is caused by the human papilloma virus (HPV) – an infection that around eight in 10 people in the UK will get and can now be vaccinated against. In the last 20 years Cancer Research UK funded clinical trials to help create the HPV vaccine, which is now offered to children across the country and expected to save many lives.
Over the next decade, as people who have been vaccinated reach the age when they’re most at risk of cervical cancer, disease rates are expected to fall. But the vaccine doesn’t protect against all types of HPV, so it’s still vital that cervical screening continues alongside.
As well as screening and vaccination, we can beat cervical cancer by knowing the warning signs to catch the disease at an early stage when treatment is most likely to work. Common symptoms are abnormal bleeding or discharge, pain during sex and pain in the pelvis. For more information visit cruk.org/about-cancer/cervical-cancer.
Busting myths and breaking barriers
- “I would know if something was wrong, I don’t need a test” Screening means testing people for early stages of a disease before they have symptoms, so even if you feel fine this doesn’t mean you don’t need to attend. Cervical screening isn’t designed to find cancer (although it sometimes does) but to look for HPV and tiny changes in cells that could become cancer, so then these abnormalities can be removed and the disease can be prevented. So you shouldn’t wait for a warning sign—but if you notice something that’s not normal for you, even if you’ve recently been for screening, tell your doctor about it. It’s probably not cancer, but it’s always worth checking out.
- “I am too young/old to be at risk” Although cancer overall is more common among over-65s, cervical cancer also affects younger people; more than half of those diagnosed each year in the UK are under the age of 45. Cervical cancer is very rare in under-25s, so screening is offered between the ages of 25 and 49 every three years, and every five years after that. It’s a personal choice, but we encourage you to read all the information and consider going for cervical screening when the invite arrives.
- “I had the HPV vaccine so I don’t need screening” HPV is the cause of almost all cervical cancers, and the vaccine protects against the two types of HPV that cause the most cases of cervical cancer—but there are other forms of the infection that it doesn’t cover, so people who have had the vaccine still need to go for screening.
- “I can’t show a stranger my private parts, screening is too awkward” Some people can find cervical screening uncomfortable, but doctors and nurses are professionals—they’ve done it hundreds of times and their focus is on protecting you, your dignity and your health. If it helps, you can specifically ask to see female staff. The NHS also offer a chaperone, or you can bring a friend if you want that support.
- “I can’t have HPV, I’ve only been with one person / used condoms etc.” HPV can be spread by skin-to-skin contact, not just penetrative sex, so it’s very easy to catch and wearing condoms only reduces the risk. 80 percent of people in the UK will get HPV in some form (there are over 100 types) and it can lie dormant for years with no symptoms—so even if you haven’t been sexually active or had a new partner for a long time, you could still have HPV.
- “I don’t have time to go for screening” It can be tough to fit doctors’ appointments into busy schedules, but cervical screening saves lives and takes mere minutes. You only have to go once every three to five years, depending on your age, so it’s a small inconvenience that can have a huge impact. Some GP surgeries and clinics stay open later to make it easier for people to attend.
- “I lead a healthy lifestyle so I won’t get cancer” Some cancers are preventable, such as those caused by smoking and excess weight, but there is still a lot we don’t fully understand about cancer risk. Although you can make lifestyle changes to stack the odds in your favour, there are no guarantees. Cervical cancer can be prevented, but this happens through vaccination and screening, not lifestyle changes.
Source: Read Full Article
