Horner syndrome is a set of symptoms affecting the eye which is thought to occur due to damage of the sympathetic nerve supply to the eye.
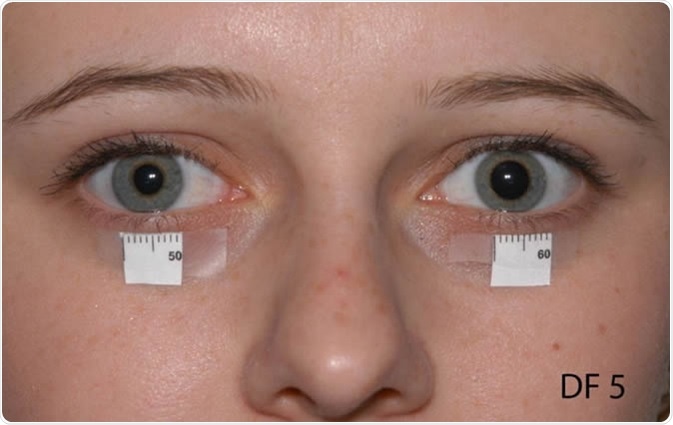
Considered to be a rare condition, Horner syndrome is characterized by facial anhidrosis (reduced sweat production over the face), partial ptosis (falling or drooping of the upper eyelid), and miosis (constricted pupil). The condition is thought to be caused by disruption in the sympathetic nerve supply as a result of nerve damage.
Anatomy of the eye
There are three different neurons which make up the nerve supply of the eye. These originate from the posterolateral hypothalamus and end as the ciliary nerves which supply the iris dilator and superior tarsal muscles. These pathways contain first, second and third-order neurons which originate from and project to different areas.
First-order neurons are found within the hypothalamus and extend through the midbrain and pons on the same side as their origin, finally ending at the spinal cord. Second-order neurons leave the spinal cord at the T1 (corresponding to the first thoracic vertebra) level and subsequently enter the cervical sympathetic chain. Finally, third- order postganglionic neurons branch into the vasomotor and sudomotor fibers which follow the external carotid artery and supply the blood vessels and sweat glands in the face.
Causes of Horner syndrome
Research has found that Horner syndrome is most often the result of local or systemic disease, or may be caused by some forms of treatment. It is sometimes congenital: individuals are born with the condition, or more rarely inherit it. in some cases patients develop the condition because of trauma, or it is acquired secondary to another disease. No cause can be found in some patients.
Since the sympathetic nerves traverse a long pathway, they may be damaged during their intracranial, extracranial or intra-orbital course. For example, the nerves that are responsible for dilating the pupils in dark environments travel in proximity to several other structures. They start in the brain, pass down the spinal cord, between the lungs and finally through the neck. If damage occurs at any point along this path, then Horner syndrome may occur. The specific cause of the syndrome is thus linked to the anatomical area of disruption.
First-order neurons
First-order neurons are most likely to be impacted by intracranial conditions such as:
- Strokes
- Meningitis
- Encephalitis
- Multiple sclerosis
- High spinal trauma and tumors
- Lateral medullary syndrome
Second-order neurons
As second-order neurons traverse the thoracic region they can be affected by conditions such as:
- Pancoast tumors (at the apex of a lung)
- Dental abscess in the mandibular region
- Mediastinal lymph gland enlargement
- Trauma to brachial plexus
- Lesions of the subclavian artery
Third-order neurons
Third-order neurons are found close to the internal carotid artery and cavernous vein, and can be affected in conditions such as:
- Cluster headaches and migraines
- Herpes zoster infections
- Temporal arteritis
- Carotid cavernous fistula
Symptoms of Horner syndrome
Horner syndrome may present with different symptoms depending on the location of the disruption in the chain of neuron transmission. However, the most common symptoms include:
- Different-colored irises on either side
- Reduction in the size of the pupil
- Drooping and/or swelling of the upper eyelid
- Sinking of the eyeball
How is Horner syndrome diagnosed?
Being able to identify the site of damage or disruption of the sympathetic nerves is important in managing the symptoms experienced. In order to do this, doctors will do a detailed examination of both eyes to see whether the syndrome is definitely present, and to determine the area of damage. Further tests may be done, including an MRI scan and X-ray of the chest to look for potential causes of the damage.
Some of the following points may need to be considered:
- A detailed medical and medication history to rule out the use of mydriatic or miotic agents
- If sensory, hearing, balance and swallowing problems are present this may indicate a central process involving the first-order neurons
- Any prior history of surgical intervention or trauma involving the back, shoulder, neck, head or face may indicate that second-order neurons are involved
- If facial numbness, double vision, pain or headaches are present, this may indicate the involvement of third-order neurons
How is Horner syndrome treated?
The treatment of patients with Horner syndrome depends on the cause and location of the lesion. For some patients, the exact cause or lesion and therefore, only symptomatic treatment is offered. If a clear cause is found, then referral to a specialist may be required to effectively treat the underlying cause.
Are there any complications of Horner syndrome?
Research suggests that the presence of Horner syndrome does not typically lead to loss of vision or damage to the eye, but may instead be evidence of damage to structures through which the nerve passes. Therefore, it is vital to identify the location of the damage and its cause, as the underlying issue may be serious. For example, a tumor in the lung and a stroke in the brain are just two conditions that have been linked to the cause of the syndrome.
Sources
- Horner Syndrome: https://www.ncbi.nlm.nih.gov/books/NBK500000/
- Horner’s Syndrome: https://mft.nhs.uk/app/uploads/sites/2/2018/04/REH-176.pdf
Further Reading
- All Horner Syndrome Content
Last Updated: Apr 28, 2019
Source: Read Full Article
