Drug-induced liver injury (DILI) is a leading reason for preclinical safety attrition and post-market drug withdrawals. Drug-induced mitochondrial toxicity has been shown to play an essential role in various forms of DILI, especially in idiosyncratic liver injury. In this study the authors examined liver injury reports submitted to the Food and Drug Administration (FDA) Adverse Event Reporting System (FAERS) for drugs associated with hepatotoxicity via mitochondrial mechanisms compared with non-mitochondrial mechanisms of toxicity.
The frequency of hepatotoxicity was determined at a group level and individual drug level. A reporting odds ratio (ROR) was calculated as the measure of effect. Between the two DILI groups, reports for DILI involving mitochondrial mechanisms of toxicity had a 1.43 (95% CI 1.42–1.45; P < 0.0001) times higher odds compared to drugs associated with non-mitochondrial mechanisms of toxicity.
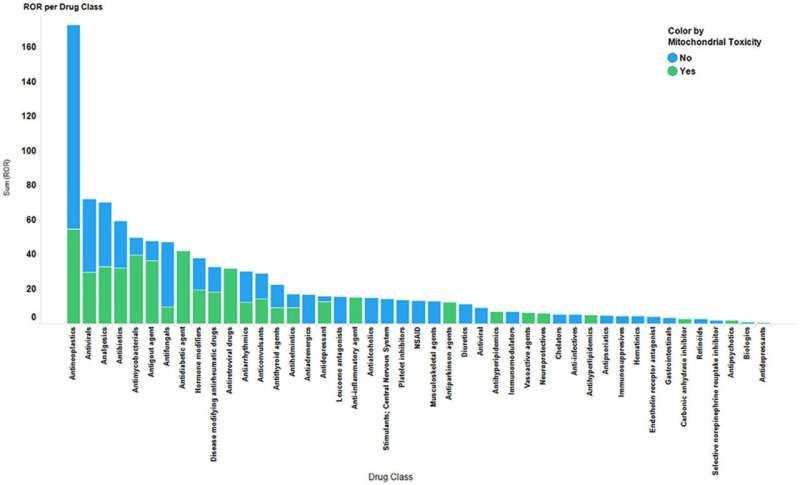
Antineoplastic, antiviral, analgesic, antibiotic, and antimycobacterial drugs were the top five drug classes with the highest ROR values. Although the top 20 drugs with the highest ROR values included drugs with both mitochondrial and non-mitochondrial injury mechanisms, the top four drugs (ROR values > 18: benzbromarone, troglitazone, isoniazid, rifampin) were associated with mitochondrial mechanisms of toxicity. The major demographic influence for DILI risk was also examined.
There was a higher mean patient age among reports for drugs that were associated with mitochondrial mechanisms of toxicity [56.1 ± 18.33 (SD)] compared to non-mitochondrial mechanisms [48 ± 19.53 (SD)] (P < 0.0001), suggesting that age may play a role in susceptibility to DILI via mitochondrial mechanisms of toxicity. Univariate logistic regression analysis showed that reports of liver injury were 2.2 (odds ratio: 2.2, 95% CI 2.12–2.26) times more likely to be associated with older patient age, as compared with reports involving patients less than 65 years of age.
Compared to males, female patients were 37% less likely (odds ratio: 0.63, 95% CI 0.61–0.64) to be subjects of liver injury reports for drugs associated with mitochondrial toxicity mechanisms.
Source: Read Full Article
